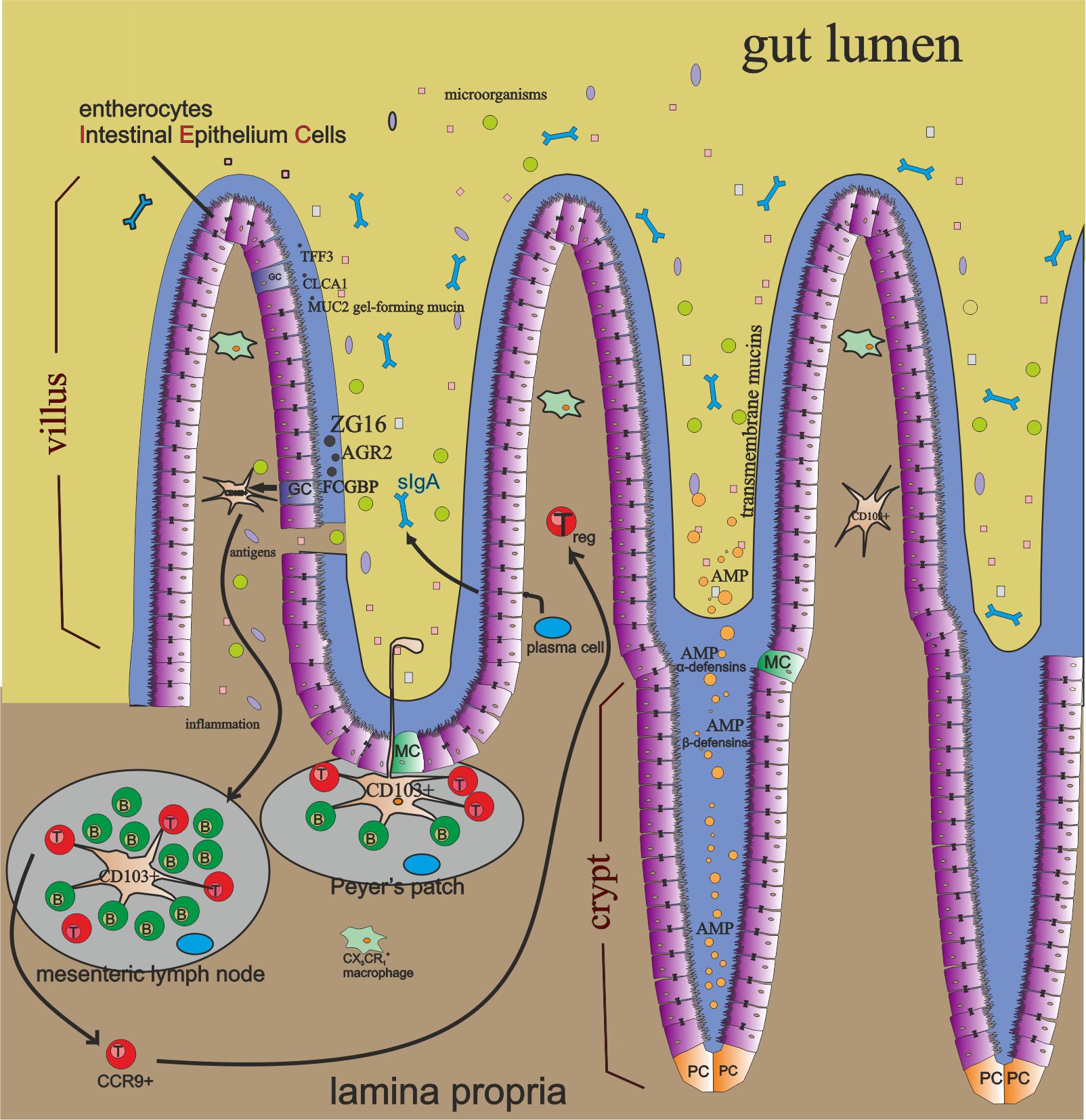
Gastrointestinal tract structure.
The digestive tract’s function is to take , digest, absorb and excrete undigested food residues. But did you know that over 70% of your immune system is localized there? Eating everyday we provide to our organism bacteria, viruses, yeast and parasites. Also possibly toxins, heavy metals or other chemicals. Constant contact of intestinal microbiome with GALT system is necessary to keep appropriate immune response. Gut is so autonomous that it has its own immune and nervous system. Immune system of a gut is a lymphatic tissue connected with intestinal mucosa membrane, so called GALT (gut associated lymphoid tissue). GALT is a part of cental lymphatic system connected with mucosa membranes, so called MALT (mucosa-associated lymphoid tissue) and provides strong local protection of the mucosa. MALT’s morphological components are masses of lymphatic tissue (lymphoid nodules) and in mucosa and submucosa layer.
Lymphatic tissue associated with GALT contains over 70% of lymphocytes of the entire immune system, in which B lymphocytes that secrete mucosa IgA antibodies are the most numerous group.
Click on the picture to enlarge. I reserve the copyright to the image. No copying or distribution without my permission.
GALT system consists of:
Physical components.
- gut microbiota – also known as commensal bacteria. They protect against harmful or pathogenic bacteria growth. They compete with bad bacteria for nutrients and release antimicrobial substances. Good bacteria also regulate the process of digestion and absorption of critical substances for organism. They are able to produce themselves short fatty acids to provide energy to protective intestine epithelial cells. They also may stimulate goblet cells to increase mucin surface thickness. The lower amount of good bacteria the thiner mucosa layer and the lower protection against pathogens’ invasion on host’s immune system. It may lead to inflammation and inflammatory diseases. Commensal bacteria or their products like lipopolysaccharide (LPS) and peptidoglycan have ability to restore mucus layer. Number of microbiota plays a big role in epithelium cells renewal. If “leaky gut occurs” bacteria in gut lumen and their products may reach lamina propria and induce inflammation. If translocated into peripheral circulation may cause tissues damage and autoimmunity.
- inner and outer layer of mucus that cover intestine epithelial cells. It’s main component is gel-forming mucin (MUC2) produced by goblet cells. Mucus contains many molecules as IgA, enzymes and proteins.
- Intestine epithelial cells (IEC) that cover as large as 400 m² surface area. Cells are renewed every 3-5 days not including Paneth cells with about two month life span. All epithelial cells are produced from intestinal stem cells that are hidden at the very bottom of Lieberkün crypts.
-
- Enterocytes – the most abundant IEC type, about 90% of all cells. Responsible for nutrients uptake and gram-positive bacteria population control by expressing antimicrobial proteins (RegIIIγ). They also produce transmembrane mucins
- Goblet cells – they produce mucin MUC2 and other mucus components. They also present antigens to dendritic cells CD103+in lamina propria in small intestine by forming goblet cell-associated antigen passages (GAPs). These cells and GAPs they create may sense and inhibit the translocation of invasive pathogens into host’s immune system.
- Paneth cells – they produce antimicrobial proteins (AMPs) : α-defensins, β-defensins, C-type lectin, cathelicidin, lysozyme, intestinal alkaline phosphatase (IAP) – may inactivate LPS, prevent it’s translocation through epithelium and may regulate Tj proteins to increase zonula occludens protein ZO-1 (Tj-1) and ZO-2 (Tj-2), Ang4 – Bacteroides thetaiotaomicron bacteria induce paneth cells to produce this AMP. Microbes interact with these substances.
- M-cells (microfold cells) – they transport (transcytose) antigens through cytoplasm across the intestinal epithelium to the Peyer’s patches localized beneath.
- Enteroendocrine cells
- Cup cells
- Tuft cells
-
- Tight Junctions (Tj) – Intestinal epithelial cells create a continous connection and are sealed by tight junctions proteins. Such a transfer of substances across the gut through spaces between epithelium cells is called paracellular permeability and may be increased by pathological conditions. Zonula occludens is one of such proteins.
Biochemical components.
These components have antimicrobial properties and exist in mucus, gut lumen and contain bile acids. Their role is protection against contact of microbes, toxins and other luminal antigens with host cells. The longer distance from stomach the pH gets higher. Of course the more colonized microbiome in intestine tract and the the more antimicrobial proteins (AMP) are being produced.
Immunological components.
- Peyer’s patches – groupings of lymphoid follicles in the mucus membrane that lines your small intestine (aggregated lymphoid nodules). They control intestinal bacteria populations and prevent pathogenic bacteria growth.
- macrophages – a type of white blood cells that reach the place of infection as first. We distinguish two types: M1 and M2. M1 stimulates immune system to fight by increasing inflammation. In a process called phagocytosis they engulf and digest unhealthy cells. But first they need to undergo biochemical processes to be activated. Activated macrophage is more cytotoxic and has a different cellular structure. M2 cells have ability to release anti-inflammatory cytokines that decrease innflammation in a body. Intestinal mononuclear phagocytes like CX3CR1+ macrophages are capable to sense luminal contents. Moreover these expressing cells may sample antigens by creating transepithelial dendrities (TEDs) structures dependantly of CX3CL1 chemokine, expressed by certain intestinal epithelium cells.
- plasma cells – reside in intestinal lamina propria and produce sIgA in amount of 50mg/kg of body daily!
- secretory IgA (sIgA) – immunoglobulin that resides mainly on intestinal mucosa surfaces and is very important to keep body protected against pathogens. In comparison with other antibody isotypes, it’s special feature is the fact that in protease-rich environment it doesn’t loose it’s resilience and stays active. Immunoglobulins sIgA may be transcytozed through epithelium and secreted in the gut lumen. Secretory IgA binds to bacteria and viruses that have got into the digestive tract and bronchi and helps to remove them from the body. As a substance secreted into intestinal lumen in a specific concentration may be intestinal indicator (marker) of gut condition.
- dendritic cells.
Leaky gut and autoimmune connection.
Translocation.
Many diseases have been associated with altered and poor intestinal microbiome (Alzheimer’s diesease, alcoholic liver disease, cancer and many autoimmune disorders), with dysbiosis, intestinal barrier dysfunction and microbial translocation. Translocation leads to production of autoantibodies against self antigens that distroy body’s own tissues. M-cells transport (transcytoze) antigens from gut lumen across intestinal epithelium to Payer’s patches in lamina propria of small intestine. Also presentation of luminal antigens to CD103+ dendritic cells by goblet cells in lamina propria is observed. Goblet cell-associated antigen passages are formed (GAPs). Goblet cells and GAPs are able to recognize pathogenic invaders and ihibit their penetration into host’s immune system.
Commensal bacteria.
Commensal bacteria and mucus layer contribute to maintenance homeostasis phenomenon. Mucus layer is rich in antimicrobial proteins (AMPs, for example RegIIIγ produced by enterocytes) that let immune system keep microbiota in check and microbiota releases some metabolic products that inhibit host’s immune system. Bacteria and their products relocation may trigger abnormal immune response. Increased permeability across epithelium induces inflammation state. Factors that trigger this gut leakiness mechanism and microbial translocation from gut lumen may be : diet, infections, alcohol consumption, burn injury, other stress etc.
How to decrease intestinal permeability and repair leaky gut?
By maintaining healthy gut, strengthening tight junction (Tj) proteins connections , support of intestinal epithelial cells renewal and increasing number of commensal bacteria to keep mucosa layer thick! Reversing leaky gut may be an atractive therapeutic strategy!
1. Optimize your diet because it’s 70% of your success! I feel the best when consume glutenfree, low in added oils and vegan – but healthy foods. Meals prepared at home, rich in fresh vegetables and fruits, not fast food labeled vegan! Click on the certain link to find something really nourishing and healthy! In the case you want to commit a small sin click here!
2. Very important Vitamin D has been recognized as a intestinal permeability protector. This vitamin induces expression of tight junction (Tj) proteins like ZO-1 and claudin-1.
3. Researchers found out that low-fiber diet consumption may trigger the overgrowth of bacteria population devastating mucus membrane thickness (Akkermansia muciniphila, Bacteroides caccae)
4. A diet rich in high saturated fats leads to decrease the number of Lactobacillus, increases Oscilibacter (extra virgin coconut oil is controversial)
5. Oscilospirra abundance weakens mucus membrane increasng permeability by forming ZO-1.
6. Stress may result in increased intestinal permeability, thus microbiome changes and populations of aerobic and anaerobic bacteria producing butyrate decreases in stool.
7. Alcohol changes the quality and quantity of microbiome, induces lipopolysaccharyde(LPS) translocation and alcoholic liver disease. Supresses Lactobacillus, disrupts mucosal integrity. Some bacteria like e.coli can produce themselves alcohol and this is the cause they are able to live in intestine. Drinking alcohol may supress activity of RegIIIγ but supplementation of Lactobacilli and Bifidobacteria may restore RegIIIγ functions. E. coli are LPS-produccing bacteria and Bifidobacterium controls them.
8. Microbiota transplantation may help rebuilt leaky gut and strenghten protection .
9. Probiotics that don’t solluble in a stomach and prebiotics – foods that feed good bacteria in a gut may reduce the intestinal permeability. The application of Bacteroides fragilis to prevent a leaky gut and reverse autoimmunity is beneficial but warrants further investigation.
10. Alive probiotics on freshly grown vegetables and fruits (this is this aspect of the theory of eating dirty foods)
11. Sprouts – help to colonize the ileum with unique bacteria
Do you like the post?
Like and follow my facebook page (https://www.facebook.com/vitaminove/). First click Like! and then set “display first” in follow options.
Also check out my Instagram (https://www.instagram.com/vitaminove_com/)
Leave a comment!
Please share with the button below!
Bibliography:
- dr n. med. Mirosława Gałęcka, “Dieta w chorobach autoimmunologicznych”, PZWL Wydawnictwo lekarskie.
- Dr n. med. B. Sieradzka, “Znaczenie układu odpornościowego przewodu pokarmowego dla organizmu“.
- Qinghui Mu, imageJay Kirby, imageChristopher M. Reilly and imageXin M. Luo,; Leaky Gut As a Danger Signal for Autoimmune Diseases.
- Arndt Manzel, Dominik N. Muller, David A. Haffler, Susan E. Erdman, Ralf A. Linker, M, Markus Kleinewietfeld, Role of Western Diet in inflammatory autoimmune diseases.
- Helena Tlaskalová-Hogenová, Renata Štěpánková, Hana Kozáková, Tomáš Hudcovic, Luca Vannucci, Ludmila Tučková, Pavel Rossmann, Tomáš Hrnčíř, Miloslav Kverka, Zuzana Zákostelská, Klára Klimešová, Jaroslava Přibylová, Jiřina Bártová, Daniel Sanchez, Petra Fundová, Dana Borovská, Dagmar Šrůtková, Zdeněk Zídek, Martin Schwarzer, Pavel Drastich & David P Funda, The role of gut microbiota (commensal bacteria) and the mucosal barrier in the pathogenesis of inflammatory and autoimmune diseases and cancer: contribution of germ-free and gnotobiotic animal models of human diseases.
- Yan Y. Lam*, Connie W. Y. Ha, Craig R. Campbell, Andrew J. Mitchell, Anuwat Dinudom, Jan Oscarsson, David I. Cook, Nicholas H. Hunt, Ian D. Caterson, Andrew J. Holmes, Len H. Storlien, Increased Gut Permeability and Microbiota Change Associate with Mesenteric Fat Inflammation and Metabolic Dysfunction in Diet-Induced Obese Mice.






Comments
Great article. Couldn’t be write far better!
Best regards,
Thomassen Raahauge
Pingback: Samoleczenie choroby autoimmunologicznej dietą i stylem życia. - vitaminove.com
Pingback: Self-healing autoimmune disease with diet and lifestyle. - vitaminove.com